How African Health System can Match Strategy with Reality
Choosing the Right Healthcare Delivery Approach
When the Right Model Saves Lives
In 2009, Ondo State, Nigeria, faced one of the highest maternal mortality rates in the country with over 745 deaths per 100,000 live births. For many women, giving birth was a gamble with their lives. Clinics were underused, skilled birth attendants were scarce, and too many expectant mothers were delivering at home without trained medical support.
Then came the Abiye (Safe Motherhood) Initiative. Instead of relying on a one-size-fits-all model, the Ondo state government, under his excellency Dr. Mimiko, took a hard look at the realities on the ground. They realized that simply building more hospitals that the average Nigerian could not afford would not work. The barriers to care were deeper: transportation challenges, cost of care, cultural preferences, and mistrust of the health system.
The solution? A diagonal approach that combined immediate maternal health interventions with systemic improvements:
Mother and Child Hospital Model offers free consultations, laboratory tests, medication, admissions, and surgeries
Community health rangers trained to track pregnancies and encourage facility deliveries
Mobile phone hotlines connecting women to emergency transport
Integration of maternal care into primary health systems so every woman, rural or urban, had a reachable care point
The results were extraordinary. By 2016, Ondo State became the only state in Nigeria that met the millennium development goal to improve maternal health with an approximate 85% reduction in maternal mortality. More women began trusting and using health facilities. The model worked because it was built for Ondo’s context while leveraging both targeted interventions and system-wide strengthening.
This is the power of choosing the right healthcare delivery approach. However, in too many parts of Africa the projects fail because the delivery model is misaligned with the community’s needs and realities.
In 2018, a well-funded health NGO launched a state-of-the-art maternal clinic in rural northern Nigeria. The equipment was world-class, the building was exquisite but within 18 months, the clinic stood nearly empty. The clinic relied on specialist physicians who were never available locally, the pricing was unaffordable for most residents, and public health outreach was nonexistent. This initiative had chosen the wrong approach for the community’s realities.
Across Nigeria and Africa at large, this story repeats itself: a mismatch between intervention design and delivery approach. At Ziora Health, we believe solving this problem starts with determining the right delivery approach for the desired impact.
The Stakes: Why Choosing the Right Model Matters
Africa faces a dual challenge: enormous health needs and constrained human and infrastructure resources.
The World Health Organization estimates up to 40% of health budgets in low- and middle-income countries (LMICs) are lost to inefficiency.
As of 2022, Sub-Saharan African countries have approximately 18 physicians per 100,000 people with disparities in physician density
Highest physician density: Cape Verde has 4.5 physicians per 1,000 people
Lowest physician density: Gambia has only 6 physicians per 100,000 people
Thus, in this environment, choosing the wrong delivery approach is expensive. Clinics sit empty, patients lose trust in health systems, and short term projects collapse after donor exit. Furthermore, structural biases exacerbate the problem as brain drain depletes the local health workforces and rural populations are often excluded from urban centered programs.
The Three Approaches to Healthcare Delivery
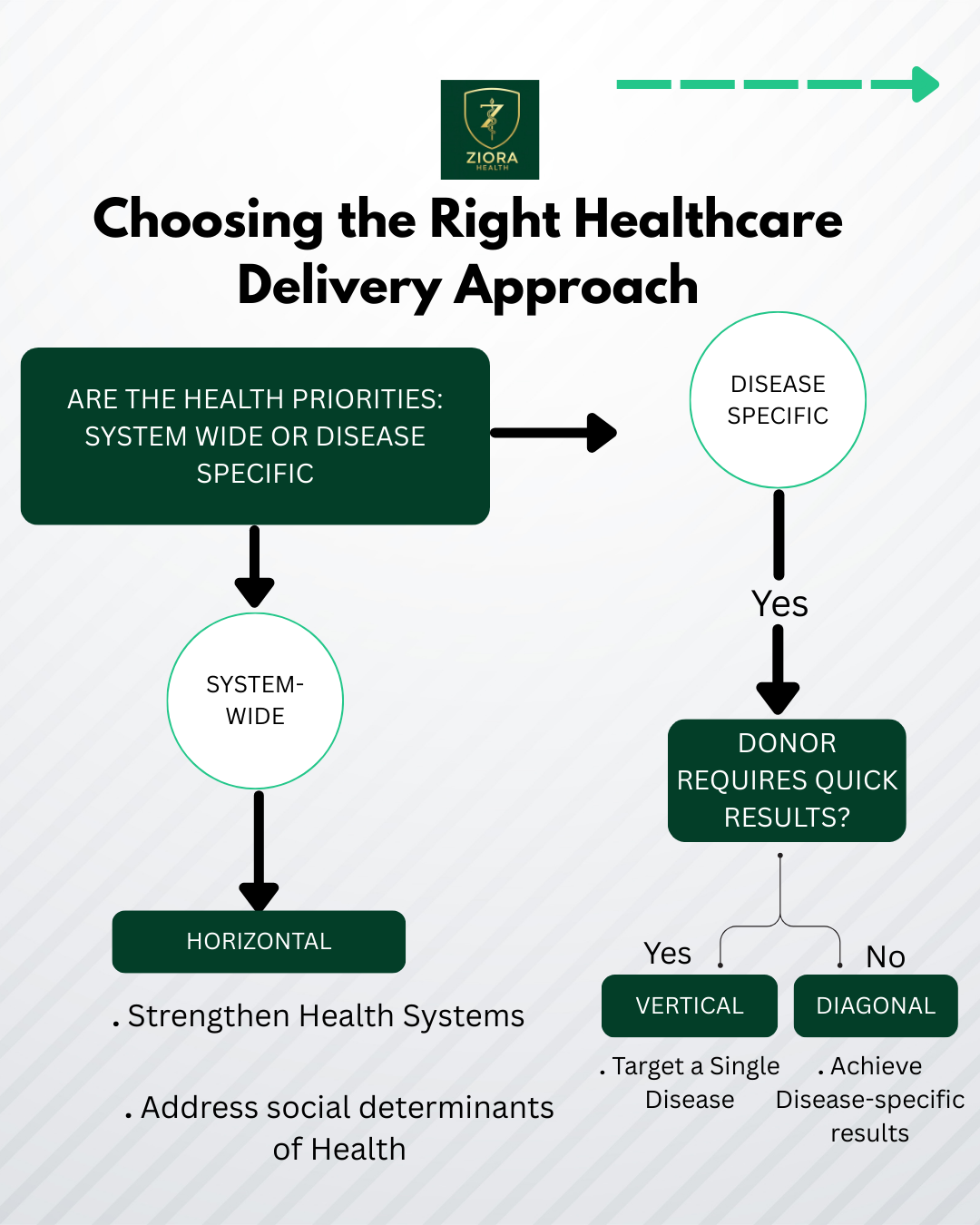
Global health funding and delivery typically follow one of three models: Horizontal, Vertical, and Diagonal . Each has its strengths, weaknesses, and ideal use cases.
1. Horizontal Approach: System Strengthening for the Long Game
A flexible, comprehensive approach that addresses the underlying, structural factors affecting health such as infrastructure, workforce, and community systems. A noteworthy example of this is the WHO’s International Health Regulations which strengthen global disease surveillance to prevent cross-border spread as a prime horizontal strategy.
Strengths:
Tackles root causes of poor health
Builds resilience to changing disease patterns
Can integrate multiple health services under one umbrella
Weaknesses:
Harder to measure short-term outcomes
Requires long timelines and sustained funding
When to Choose It:
When your goal is long-term, system-wide impact
When diseases or challenges are multifactorial (e.g., maternal mortality, health workforce shortages)
2. Vertical Approach: Targeted Wins Quickly
A focused, disease-specific approach delivering measurable results through specialized programs or technology. A famous example is the smallpox vaccination campaigns which tracked immunization rates through robust epidemiological surveillance.
Strengths:
Delivers rapid, visible results
Easier to secure funding (donors love measurable outcomes)
Can address urgent or high-burden diseases efficiently
Weaknesses:
Risks neglecting broader system needs
Often dependent on short-term funding cycles
May collapse if donor interest wanes
When to Choose It:
For outbreak response or diseases with clear, singular interventions
When donor timelines demand fast results
3. Diagonal Approach: The Best of Both Worlds
Uses disease-specific interventions to also strengthen the broader health system. Mexico’s vitamin A supplementation campaign is a perfect example as it reduced childhood blindness while integrating vitamin A distribution into the primary healthcare system.
Strengths:
Addresses immediate health needs
Leaves behind stronger systems
More sustainable than vertical alone
Weaknesses:
Requires strong coordination between disease programs and health systems
Can be complex to implement as it depends on government involvement
When to Choose It:
When you want measurable short-term impact without sacrificing long-term resilience
Ziora Health Framework for Choosing the Right Approach
Through our work with African health systems, we’ve developed a five-pillar decision framework to guide ministries, non governmental organizations and private providers in selecting the right delivery model.
Pillar 1: Access Alignment
Ask: Who is your target patient population? How will they reach you?
Use geo-mapping to assess proximity, transportation options, and urban vs rural distribution.
Case Insight: Mobile clinics in Kenya were successful for cataract surgeries since they are elective procedures; however, mobile clinics failed for chronic hypertension management due to follow-up challenges.
Pillar 2: Cost Logic
Ask: Can patients afford this model without catastrophic spending?
A major barrier to care is cost so keeping in mind the economic realities of the average person is ideal to maximize intervention utilization.
Pillar 3: Workforce Reality
Ask: Do you have the human resources to sustain this model?
In the age of rapid healthcare workforce drain from Sub-Saharan Africa to the global north it is more important now than ever before to avoid models requiring specialists that are unavailable locally.
Pillar 4: Technology Fit
Ask: Will technology help or hinder your delivery?
Tele-psychiatry in Sub-Saharan Africa works when platforms are low-bandwidth optimized and has translation services available in local languages.
Pillar 5: Sustainability Lens
Ask: Will this model still work in five years?
It is vital that the model incorporates integration to primary care, community ownership, and recurrent funding streams from local governments.
Applying the Framework: Tele-psychiatry in West Africa
Scenario: A nonprofit wants to launch tele-psychiatry in Ghana and Nigeria.
Access Alignment: Internet penetration is ~70% in Ghana, but only 50% in rural Nigeria thus hybrid hubs may be needed.
Cost Logic: Mobile payment integration (M-Pesa, MTN Money) can lower cost barriers.
Workforce Reality: Leverage diaspora psychiatrists licensed to practice virtually.
Technology Fit: Low-bandwidth platforms with offline functionality for follow-ups.
Sustainability Lens: Integrate into national health insurance schemes.
Outcome: A diagonal approach that utilizes psychiatrists in the diaspora to meet urgent mental health needs while training primary care providers for on-the-ground support would be the optimal choice.
Ziora Health Call to Action
For funders: Stop prioritizing speed over sustainability.
For implementers: Choose your delivery model with as much rigor as your medical intervention.
For policymakers: Build regulatory and financing systems that allow flexible, locally adapted delivery models.
At Ziora Health, we envision an Africa where delivery models are context-driven, equity-focused, and designed to last.